
Patients from all disciplines of medicine frequently report symptoms of bloating. Other studies have shown that over 90% of patients with irritable bowel syndrome (IBS) have symptoms of bloating.
Bloating that persists or seems to manifest only after eating certain foods could mean you’re sensitive to FODMAPs, a group of carbohydrates found abundantly in many plant foods.
Foods that produce gas in one person may not cause gas in another. Some common bacteria in the large intestine can destroy the hydrogen that other bacteria produce. The balance of the two types of bacteria may explain why some people have more gas than others.
Everyone has gas and eliminates it by burping or passing it through the rectum. However, many people think they have too much gas when they really have normal amounts. Most people produce about 1 to 3 pints a day and pass gas about 14 times a day.
Gas is made primarily of odorless vapors – carbon dioxide, oxygen, nitrogen, hydrogen, and sometimes methane. The unpleasant odor of flatulence comes from bacteria in the large intestine that releases small amounts of gases that contain sulfur.
What Are FODMAPs?
FODMAP stands for fermentable oligosaccharides, disaccharides, monosaccharides, and polyols. These short-chain carbohydrates and sugar alcohols include:[1]
- Fructans
- Fructose
- Galactans
- Lactose
- Mannitol
- Sorbitol
- Xylitol
During digestion, enzymes break the bonds in carbohydrate molecules so that they can be absorbed in the small intestine. The degree to which this happens with FODMAPs varies from person to person, and the sugars that don’t get broken down travel to the colon intact, pulling water into the intestines along the way.[2] Inside the colon, gut bacteria quickly ferment FODMAPs and produce gasses such as hydrogen, carbon dioxide, and methane.
FODMAP Sensitivity Symptoms
- Gas
- Bloating
- Abdominal pain
- Visible abdominal distention
- Diarrhea
- A feeling of fullness after eating small amounts of food
Because FODMAPs are fermented in the colon, it can take anywhere from several hours to a couple of days for symptoms to manifest after consuming high-FODMAP foods.
If you suspect you’re sensitive to FODMAPs, keeping a food diary for several weeks is the best way to monitor symptom patterns and identify suspect foods.
The Low-FODMAP Diet
Cutting down on FODMAPs can be beneficial for people with IBS and others who exhibit symptoms of sensitivity. Consuming fewer FODMAPs minimizes the amount of water drawn into the intestines during digestion and reduces fermentation action in the gut. One specific protocol, developed by Monash University with the goal of controlling IBS symptoms, has three stages:[8]
Strict FODMAP restriction: 2 to 6 weeks
Reintroduction of one FODMAP food at a time: 8 to 12 weeks
Personalizing FODMAP consumption based on tolerance: ongoing
Up to 86% of IBS sufferers who stick with the diet experienced improvements in their symptoms.[9] The diet has also been used to address other functional gastrointestinal disorders, as well as specific conditions like small intestine bacterial overgrowth (SIBO).
Reducing FODMAPs When Eating Plant-Based
Following a low-FODMAP regimen can be a challenge on a plant-based diet because so many common foods are inherently high in these sugars. A food is considered “high FODMAP” if it contains more than a predefined amount[10] of oligosaccharides, disaccharides, monosaccharides, or polyols, and some of the biggest offenders are staples in many plant-based meals.[11]
Foods highest in FODMAPs include: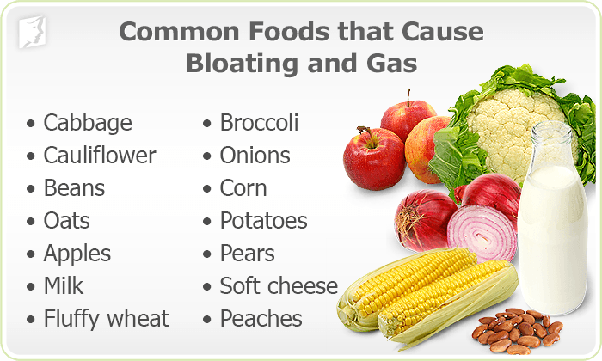
Fruits: apples, pears, peaches, cherries
Vegetables: broccoli, beets, cauliflower, garlic, mushrooms, potatoes
Beans and legumes: lentils, kidney beans, chickpeas, soya
Grains: wheat, barley, rye
Nuts: almonds, cashews, pistachios[12]
There are, however, many low-FODMAP alternatives:
Fruits: blueberries, cantaloupe, oranges, strawberries, unripe bananas
Vegetables: bok choy, peppers, spinach, sweet potatoes, tomatoes, zucchini
Grains: corn, oats, rice, quinoa, sorghum
Soy products: tempeh, firm tofu
Nuts and seeds: macadamia nuts, peanuts, walnuts, pumpkin seeds
This list is by no means comprehensive, and not all foods on the high-FODMAP list are completely off-limits. Some only trigger symptoms, when eaten in large quantities and processing methods such as canning or sprouting, can also reduce FODMAP levels.[13]
Bloating that doesn’t go away or gets worse may be the result of another condition, so continue to monitor your symptoms, and let your doctor know about any unusual or uncomfortable changes.
Remedies for Bloating (Gas)
Activated Charcoal
1/2 teaspoon of charcoal powder and gas is gone 20 minutes later. Gas is caused by fermenting foods and charcoal absorbs it all.
Anise Seeds
Pop a tsp of anise seed into the mouth and chew it thoroughly, swallow it. It will completely stop the gassiness, and very quickly
Apple Cider Vinegar
Take a Tablespoon of apple cider vinegar mixed with warm water and sipped on that until it was gone.
Baking Soda
Drinkk baking soda (1/2 teapoon) and water (1/2 cup), within 5 minutes you will feel 75% better!!!
Dietary Changes
If your stomach is distended after foods, you probably suffer from flatulence, it means you have excessive of stomach gas. One of the causes of flatulence is because you eat too much food stuff that cause stomach gas.
Here are the list of foods that give flatulence: Any Bean, fruits such as melon, honeydews, pear. , Cabbage, brocolli, cauliflower, Fatty food, Gassy drink, Tea and coffee with milk
Oregano Oil
Take a capsule of oil of oregano twice a day with meals.
References
- Gunnars, Krist. “FODMAP 101: A Detailed Beginner’s Guide.” Healthline. https://www.healthline.com/nutrition/fodmaps-101#definition.
- Warmflash, David. “Fermentable Foods: Trouble in Your Diet.” ChemMatters Online. https://www.acs.org/content/acs/en/education/resources/highschool/chemmatters/past-issues/archive-2014-2015/fodmap-intolerance.html.
- Barrett, Jacqueline S., and Peter R. Gibson. “Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols (FODMAPs) and Nonallergic Food Intolerance: FODMAPs or Food Chemicals?” Therap Adv Gastroenterol. 2012 Jul;5(4):261-8. doi:10.1177/1756283X11436241.
- Cunha, John P. “Low FODMAP Diet for IBS: List of Foods to Eat and Foods to Avoid.” MedicineNet. https://www.medicinenet.com/low_fodmap_diet_list_of_foods_to_eat_and_avoid/article.htm.
- Timing of Symptoms and FODMAPs.” Monash University. https://www.monashfodmap.com/blog/timing-of-symptoms.
- De Giorgio, Roberto, Umberto Volta, and Peter R. Gibson. “Sensitivity to Wheat, Gluten, and FODMAPs in IBS: Facts or Fiction?” Gut 65, no. 1 (06, 2015): 169-78. doi:10.1136/gutjnl-2015-309757.
- Perazzini, Suzanne. “The 8 Symptoms of FODMAP Malabsorption Explained.” The Low Fodmap Diet. September 15, 2018. https://www.strandsofmylife.com/8-symptoms-low-fodmap-intolerance-explained/.
- “Starting the FODMAP Diet.” Monash University. https://www.monashfodmap.com/ibs-central/i-have-ibs/starting-the-low-fodmap-diet/.
- Nanayakkara, Wathsala, Paula Skidmore, Leigh O’Brien, Tim Wilkinson, and Richard Gearry. “Efficacy of the Low FODMAP Diet for Treating Irritable Bowel Syndrome: The Evidence to Date.” Clin Exp Gastroenterol. 2016 Jun 17;9:131-42. doi:10.2147/ceg.s86798.
- Rossi, Megan. “10 Foods High in FODMAPs (and What to Eat Instead).” Healthline. https://www.healthline.com/nutrition/foods-high-in-fodmaps#section1.
- Gunnars, Kris. “FODMAP 101: A Detailed Beginner’s Guide.” Healthline. https://www.healthline.com/nutrition/fodmaps-101#high-fodmap-foods.
- “What Nuts Are Low FODMAP?” A Little Bit Yummy. December 18, 2018. alittlebityummy.com/what-nuts-are-low-fodmap.
- “Low-FODMAP Diet for Vegans.” Vegan Health. veganhealth.org/low-fodmap-diet-for-vegans.
Hill, Peta, Jane Muir, and Peter Gibson,. “Controversies and Recent Developments of the Low-FODMAP Diet.” Gastroenterol Hepatol (N Y). 2017 Jan; 13(1): 36–45. www.ncbi.nlm.nih.gov/pmc/articles/PMC5390324/.
